The landscape of healthcare has dramatically changed since the onset of the COVID-19 pandemic. E-visits have replaced traditional Doctor’s offices visits. Mobile devices are the norm now that quarantines have pushed the fast forward button on the adoption of telemedicine.
Before the pandemic, Telemedicine use was limited. Lower-level services, such as diabetic teaching and hospital-based specialty visits in rural areas, were its domain. Although accepted in theory, providers and patients alike were slow to warm up to virtual care. Medicare only covered telemedicine visits in very limited situations; reimbursement rates from both government and private payers were very low.
And then along came COVID-19.
Everything changed. Telemedicine guidelines relaxed.
The Centers for Medicare and Medicaid Services (CMS) began paying for telemedicine visits at the same rate as in-person visits. They relaxed many rigid guidelines which made virtual visits more accessible for Medicare patients.
Private insurance companies quickly followed suit, which led to an onslaught of new telehealth visits. The Wall Street Journal reported that CMS telemedicine visits increased from 100,000 to 300,000 per week as of March 28, 2020, with an expectation that it will continue to grow at a steady rate.
Frost and Sullivan research reported total telemedicine visits increased by 50% nationwide, and expected to hit nearly 1 billion by the end of 2020.
The question remains: what will happen when the COVID-19 crisis is over? No one knows how many of the new telemedicine administrative guidelines and reimbursement rates will remain in effect. Yet, it appears safe to say that virtual visits will remain a viable treatment option.
Virtual healthcare aligns well with the value-based-care mandate. If that continues, providers and payers will find great value in quality care which boasts efficiencies and lowers costs. Patients appreciate the convenience of receiving healthcare when and where they choose, without wait times, missed work, or transportation complications.
The Genie’s Out of the Bottle.
Seema Verman told the Wall Street Journal just that. A CMS administrator, Verma was adamant. “… the advent of telehealth has been completely accelerated. It’s taken this crisis to push us to a new frontier, but there’s absolutely no going back.”
In short, telemedicine is here to stay.
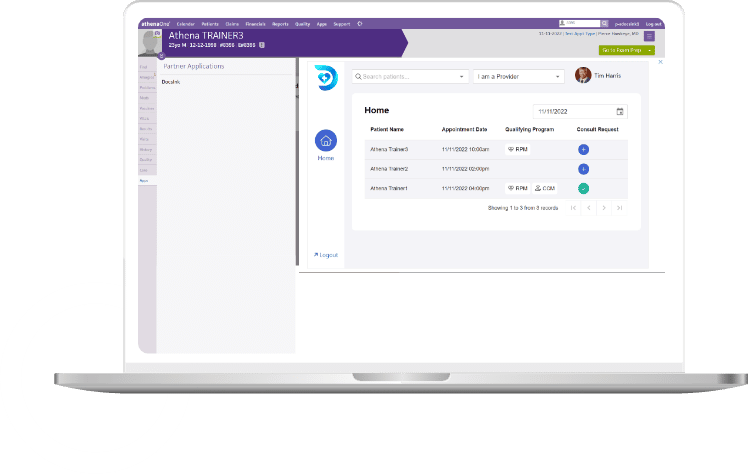
Who is DocsInk
DocsInk differentiates its software from the competition by simultaneously addressing the fiscal, communication, and connectivity needs of medical professionals. Delivered as Software-as-a-Service (“SaaS”), DocsInk is improving the way technology integrates with the various workflows of the healthcare industry. By utilizing the SMART on FHIR platform and protocols, DocsInk has set its platform to create truly integrated and system agnostic services with EHR/PM systems. Beyond our technology, that is native to Mac, PC, iOS, and Android, our team is dedicated to providing customer support and a user experience that is second to none.
Today, DocsInk provides simple, effective solutions that improve the speed, efficiency, accuracy, and adaptable methods in the delivery of patient care not just as a Telehealth Solution but also Remote Patient Monitoring (RPM), Chronic Care Management (CCM) and Mobile Charge Capture. To learn more visit us at www.DocsInk.com.