The healthcare industry continues to navigate the challenges caused by COVID-19. Clinicians are working tirelessly to provide high-quality care via Telehealth rather than face to face. Yet it seems that now, more than ever, there is a need for simple, secure, and reliable technology to connect patients to their care teams.
To that end, telehealth services guidelines have been relaxed. The Centers for Medicare and Medicaid Services (CMS), State Medicaid programs, and many major insurance payers including Blue Cross Blue Shield and United Healthcare have responded. This does two things: firstly, it simplifies reimbursement, and secondly, it expands patient access to care.
Telehealth changes
On March 6, 2020, CMS began paying physicians and qualified non-provider professionals (QPPs) for all telehealth visits. For example, 80 additional codes were added for use during the public health emergency.
Meanwhile, there are other highlights of note:
- Telehealth is now available to HPSA areas (federally defined rural areas);
- Patients may receive telehealth visits at home;
- Providers can get paid as they would if the patient was in the office;
- CMS will not include “established patient” audits with the billing provider. This allows clinicians to bill for medical services for new patients.
Here is another conundrum. Telehealth services are typically subject to CMS’ standard co-insurance and deductible amounts. As a result, Medicare patients can be left with a balance due. However, reducing the amounts owed by Medicare beneficiaries can violate the Federal Anti-Kickback Statute, the civil monetary penalty rule, and exclusion laws.
Consequently, new guidance has been issued. The Health and Human Services (HHS) Office of Inspector General (OIG) has determined that providers should not be subject to these sanctions. This allows for reduced or eliminated beneficiary cost share for telehealth or e-visits.
In addition, CMS is recognizing new virtual check-in codes for communication-based technology services (CBTS). These CBTS codes include remote evaluation of pre-recorded patient information (CPT code G2010) and virtual check-ins (CPT code G2012). Each has an average allowable amount of between $12 – $15.
New Resources
CMS has published two valuable resources. We recommend both: General Medicine Telehealth and Telemedicine Toolkit; and Medicare Learning Network (MLN) Booklet on Telehealth Services. They offer details on telehealth services and billing requirements in response to the COVID-19 health crisis.
One last recommended reading: COVID-19 State Medicaid & CHIP Telehealth Toolkit. Released in April, its goal is to expand telehealth services as the preferred means of delivering and receiving healthcare.
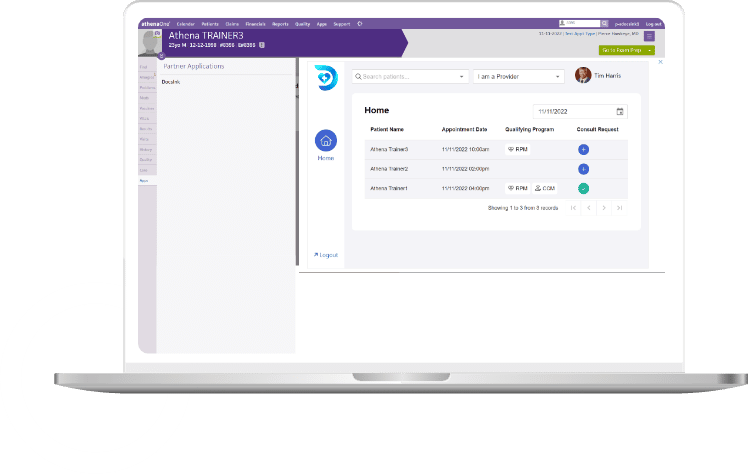
Who is DocsInk
DocsInk differentiates its software from the competition by simultaneously addressing the fiscal, communication, and connectivity needs of medical professionals. Delivered as Software-as-a-Service (“SaaS”), DocsInk is improving the way technology integrates with the various workflows of the healthcare industry. By utilizing the SMART on FHIR platform and protocols, DocsInk has set its platform to create truly integrated and system agnostic services with EHR/PM systems. Beyond our technology, that is native to Mac, PC, iOS, and Android, our team is dedicated to providing customer support and a user experience that is second to none.
Today, DocsInk provides simple, effective solutions that improve the speed, efficiency, accuracy, and adaptable methods in the delivery of patient care not just as a Telehealth Solution but also Remote Patient Monitoring (RPM), Chronic Care Management (CCM) and Mobile Charge Capture. To learn more visit us at www.DocsInk.com.